To understand better the complexity of the wound healing process and relative diseases, such as psoriasis, experimental models have been developed, both in vivo and in vitro.
In general, in vivo models for studying wound repair use mostly laboratory animals, specifically rats, mice, rabbits and pigs, each offering advantages and shortcomings. The animal that will be chosen depends on several factors, such as cost, availability, ease of handling, investigator familiarity, and similarity to humans. Traditionally, a wound experiment involves wounding the animal and monitoring gradually the wound closure. However, the protocols for the animal testing should follow the principles of the 3Rs (replacement, reduction and refinement), that verify the animal welfare. The animal model provides valuable information regarding skin biology and human pathophysiology, but has its own limitations. For instance, there are differences in skin structure and wound healing time between rodents and humans. Furthermore, these animal models are also utilized to evaluate the effect of several factors, such as nutrition supplements and medications, on wound healing.
To study chronic wounds, emerged from impaired wound healing, animal models have been developed from an acute wound by inducing diabetes, mechanical pressure or ischemia. By contrast, acute wounds have been more extensively analyzed via well-established models, such as the excisional, incisional, and burn model. All these models are summarized in Table 2.5.1M (more 2.5.1).
- Incisional wound model
The incisional skin healing model, the second most frequently employed model, can be beneficial for studying the wound tensile strength (Fig. 2.5.1). Incisional wounds are generally full thickness and scalpel induced by using a blade, that causes bleeding but minimal tissue damage, or an electrocautery or laser surgical device. This type of wound can be subdivided into primary and secondary closure model. The basic difference between these two models of closure is the use of suture in the primary model to close the wound margins. The primary closure model (or first intention) of incisional wound is ideal for biomechanical analysis of wound strength, whereas the second model (second intention) is better suited for investigating scarring at late time points. However, the size, periodicity, and type of suture used has been shown to importantly affect the tensile forces across a sheet of wounded skin. Figure 2.5.1 Incisional wound model. Τwo incisions are made on the mouse back along the paramedian (pre-operative marking), allowing tensile strength measurements by tensiometry. Adapted from: link.
Figure 2.5.1 Incisional wound model. Τwo incisions are made on the mouse back along the paramedian (pre-operative marking), allowing tensile strength measurements by tensiometry. Adapted from: link. - Excisional wound model
Excisional wound models are the most commonly used owing to their similarity with the acute clinical wounds. Since the wound edges are not sutured, they are considered as secondary closure models. Excisional wounds are generated through the surgical removal of all skin layers (epidermis, dermis, and subcutaneous fat) from the animal. Excisional wound models provide valuable information. The wound healing rate measures how the wound area closes relative to the original dimensions through photographs. The simplest method of determining wound area is by using a ruler, or other accurate scale, photographed near the wound, enabling the user to calibrate the software for the analysis. The average diameter of the wound, expressed as percentage, over the time period (Day 0 diameter/Day X diameter) is depicted in the wound closure curve (Fig. 2.5.2). The ability to generate more than one wounds in each animal increases the statistical value of this model. In addition, the wound bed is easily accessed, allowing agents, such as biomaterials and pharmaceuticals, to be tested for their effect on the repair process.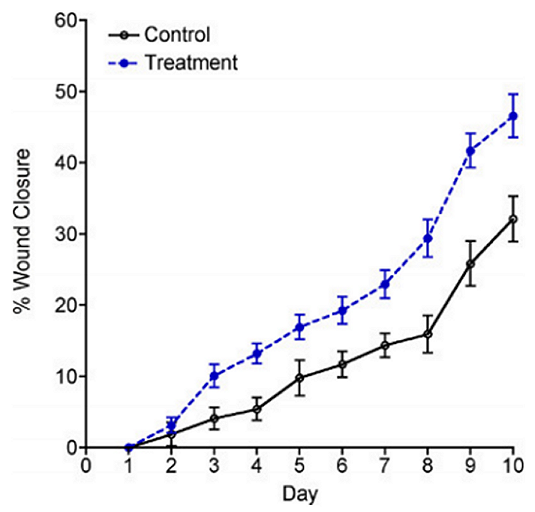 Figure 2.5.2 Wound closure graph. A therapeutic compound or vehicle control was applied to the wound bed on a daily basis (link).
Figure 2.5.2 Wound closure graph. A therapeutic compound or vehicle control was applied to the wound bed on a daily basis (link). - Burn skin models
In burn skin healing models, full- or partial-thickness wounds are generated by four different methods, hot water, hot metal tools, electricity, and heated paraffin. Different species, such as mouse, rat, pig, rabbit and dog, can be utilized as experimental burn injury models, each with its own advantages and limitations. Before the burn injury, animals are anesthetized usually with a mixture of ketamine/xylazine, the back of the mouse is shaved using a hair clipper and then hair removal cream is applied to remove the hair completely. The first model, known as water scald model, uses a template with an aperture, through which part of the body is immersed into a water bath with controlled temperature. The second method involves a hot metal plate, which directly apply heat to the skin, producing partial thickness wounds (Fig.2.5.3). In both models, the blister can be de-roofed, exposing the dermis and leaving the wound opened. To produce third-degree burn injuries, the aforementioned hot metal plate or an electric coil are utilized as these devices reach high temperatures, 170℃ and 400℃ respectively.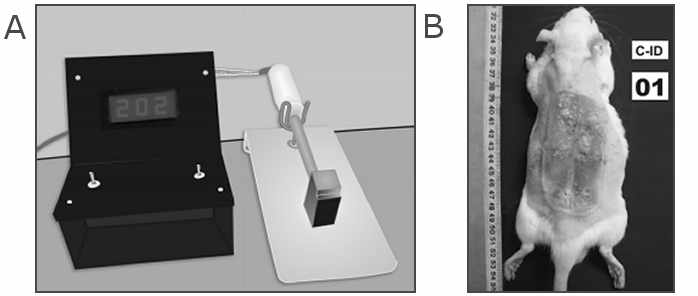 Figure 2.5.3 Burn wound model. (A) The experimental wounds were generated using this burn device with the metal plate. (B) Initial burn injury on dorsal surface of the rat. Adapted from link.
Figure 2.5.3 Burn wound model. (A) The experimental wounds were generated using this burn device with the metal plate. (B) Initial burn injury on dorsal surface of the rat. Adapted from link.
In the context of psoriasis, apart from these "normal" laboratory animals, animals with spontaneous mutations and genetically modified animals with artificially introduced mutations are also used. In addition, xenograft models, generated by transplantation of human skin fragments to immunodeficient mice, are another useful experimental model that resemble the clinical manifestations of psoriasis. Currently, imiquimod (IMQ)-induced skin inflammation is the most widely accepted psoriasis animal model since imiquimod treatment exert similar cytokine expression patterns, histopathological alterations and cellular infiltrates as those observed in psoriatic patients. All these models have been developed to study the pathophysiology of the disease, such as the aetiologia of the increased wound healing rate, as well as the effect of potential therapeutic targets.






